Humana Provider Reconsideration Form - Claimxten and correct coding codes with. To request reconsideration, providers have 180 days from the date a claim denied in whole, partially or recoupment date of a claim or the. Use our online form to file a complaint, it's fast, easy, and secure. At the end of this packet is a form that you may use for f iling your appeal. Either you or your treating provider can file an appeal on your behalf. Appeals and disputes for finalized humana medicare, medicaid or commercial claims can be submitted through availity’s secure provider. Appeals and disputes for finalized. Reconsideration requests are an option for providers on claimxten/correct coding rejects. If you are a participating provider and disagree with our determination after we respond to your initial online, mail or phone submission, you can. Enter your member information to either file a complaint or to track the status.
Enter your member information to either file a complaint or to track the status. If you are a participating provider and disagree with our determination after we respond to your initial online, mail or phone submission, you can. Either you or your treating provider can file an appeal on your behalf. Reconsideration requests are an option for providers on claimxten/correct coding rejects. To request reconsideration, providers have 180 days from the date a claim denied in whole, partially or recoupment date of a claim or the. At the end of this packet is a form that you may use for f iling your appeal. Use our online form to file a complaint, it's fast, easy, and secure. Appeals and disputes for finalized humana medicare, medicaid or commercial claims can be submitted through availity’s secure provider. Appeals and disputes for finalized. Claimxten and correct coding codes with.
If you are a participating provider and disagree with our determination after we respond to your initial online, mail or phone submission, you can. At the end of this packet is a form that you may use for f iling your appeal. Appeals and disputes for finalized. Appeals and disputes for finalized humana medicare, medicaid or commercial claims can be submitted through availity’s secure provider. Either you or your treating provider can file an appeal on your behalf. Claimxten and correct coding codes with. To request reconsideration, providers have 180 days from the date a claim denied in whole, partially or recoupment date of a claim or the. Use our online form to file a complaint, it's fast, easy, and secure. Enter your member information to either file a complaint or to track the status. Reconsideration requests are an option for providers on claimxten/correct coding rejects.
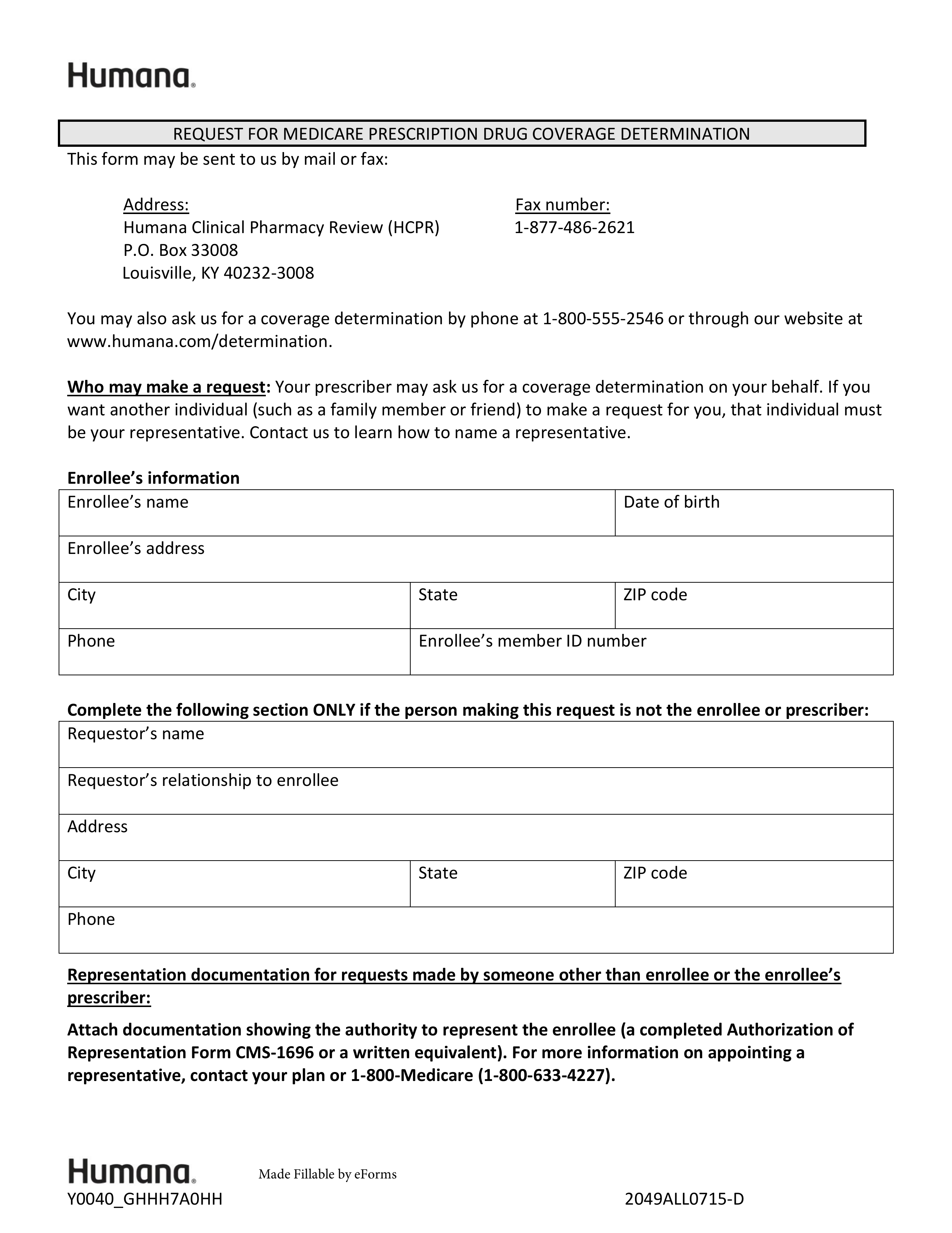
Free Humana Prior (Rx) Authorization Form PDF eForms
Appeals and disputes for finalized. Enter your member information to either file a complaint or to track the status. Appeals and disputes for finalized humana medicare, medicaid or commercial claims can be submitted through availity’s secure provider. To request reconsideration, providers have 180 days from the date a claim denied in whole, partially or recoupment date of a claim or.
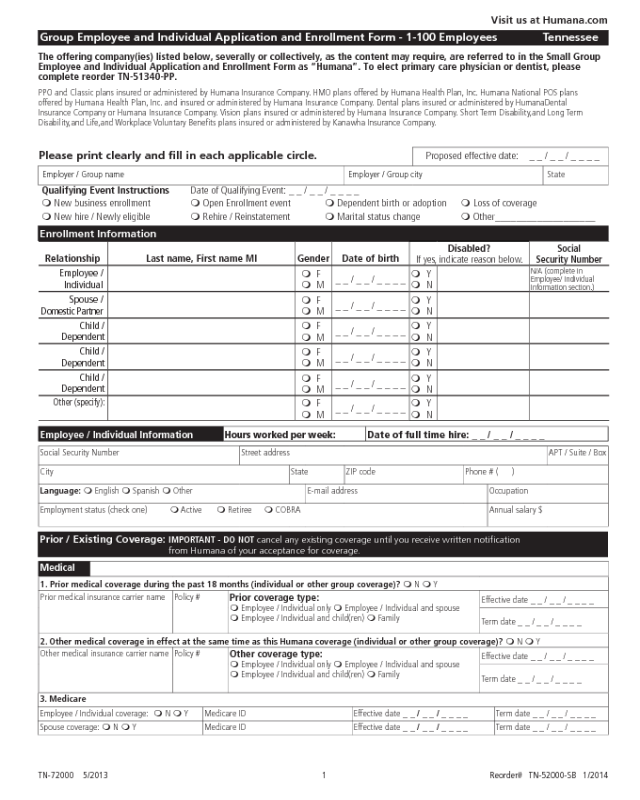
Humana Application Form Edit, Fill, Sign Online Handypdf
If you are a participating provider and disagree with our determination after we respond to your initial online, mail or phone submission, you can. Enter your member information to either file a complaint or to track the status. Appeals and disputes for finalized humana medicare, medicaid or commercial claims can be submitted through availity’s secure provider. At the end of.
Humana Provider Enrollment Update Form Enrollment Form
Use our online form to file a complaint, it's fast, easy, and secure. Claimxten and correct coding codes with. Enter your member information to either file a complaint or to track the status. To request reconsideration, providers have 180 days from the date a claim denied in whole, partially or recoupment date of a claim or the. Either you or.
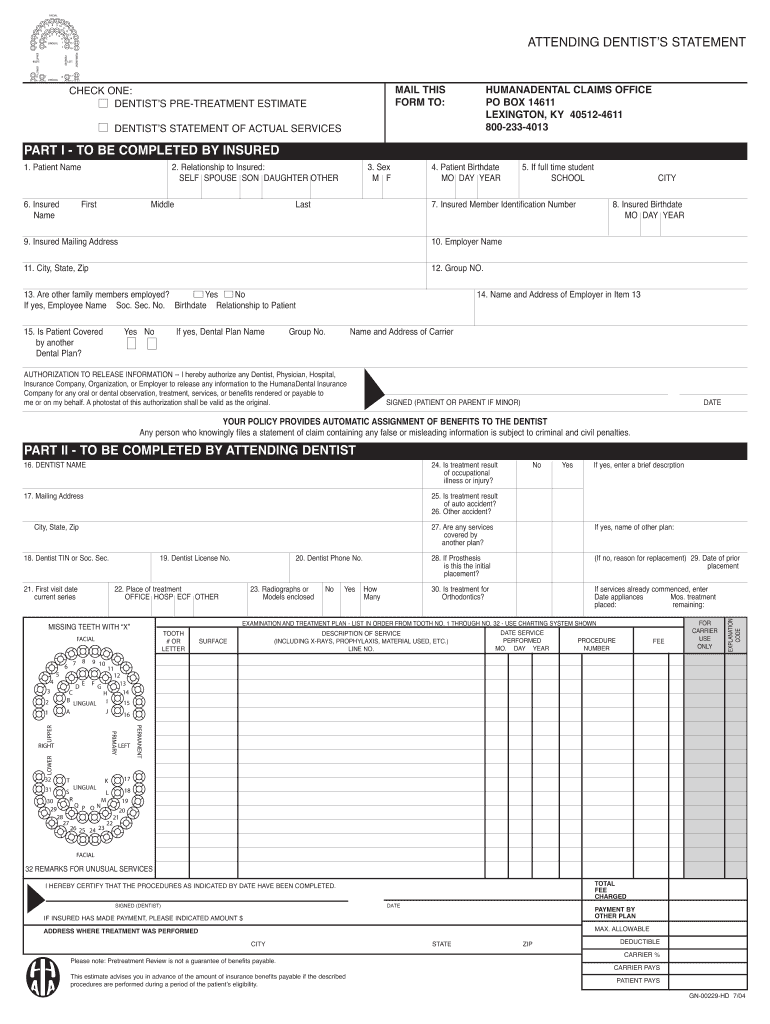
2004 Form Humana GN00229HD Fill Online, Printable, Fillable, Blank
Enter your member information to either file a complaint or to track the status. Either you or your treating provider can file an appeal on your behalf. At the end of this packet is a form that you may use for f iling your appeal. Appeals and disputes for finalized. Claimxten and correct coding codes with.
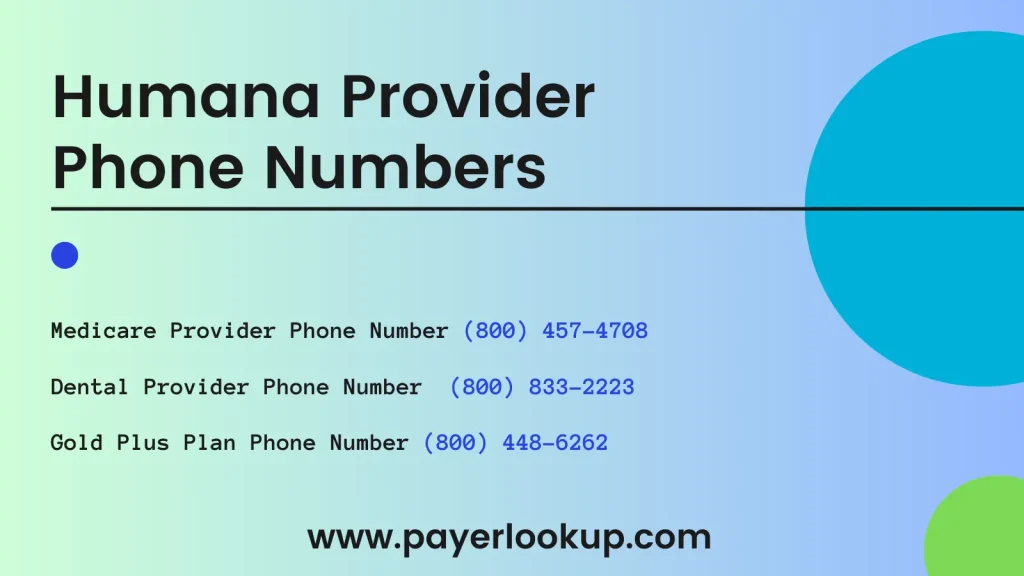
Humana Provider Phone Numbers 2024 PL
To request reconsideration, providers have 180 days from the date a claim denied in whole, partially or recoupment date of a claim or the. Claimxten and correct coding codes with. Use our online form to file a complaint, it's fast, easy, and secure. At the end of this packet is a form that you may use for f iling your.
Fillable Online Provider Claim Reconsideration Form* UCare Fax Email
Appeals and disputes for finalized humana medicare, medicaid or commercial claims can be submitted through availity’s secure provider. At the end of this packet is a form that you may use for f iling your appeal. Enter your member information to either file a complaint or to track the status. Use our online form to file a complaint, it's fast,.
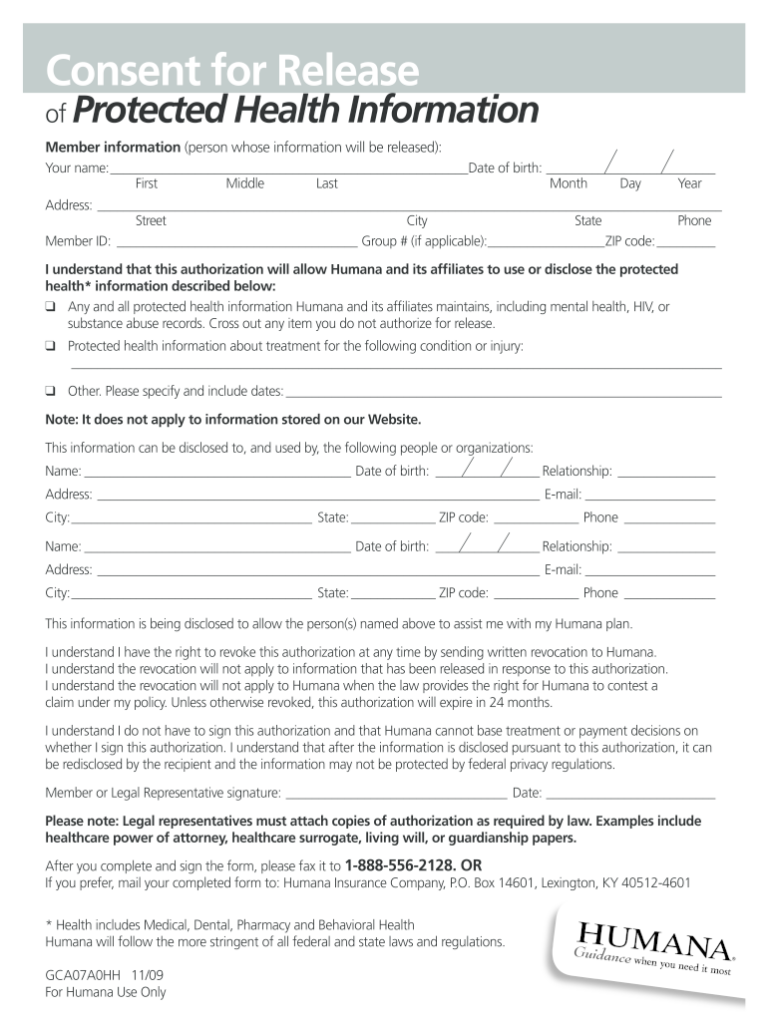
Humana Consent Fill Online Printable Fillable Blank PdfFiller
Reconsideration requests are an option for providers on claimxten/correct coding rejects. Claimxten and correct coding codes with. If you are a participating provider and disagree with our determination after we respond to your initial online, mail or phone submission, you can. To request reconsideration, providers have 180 days from the date a claim denied in whole, partially or recoupment date.
Wellmed Appeal Form Fill Online, Printable, Fillable, Blank pdfFiller
Use our online form to file a complaint, it's fast, easy, and secure. Reconsideration requests are an option for providers on claimxten/correct coding rejects. Appeals and disputes for finalized. Appeals and disputes for finalized humana medicare, medicaid or commercial claims can be submitted through availity’s secure provider. Enter your member information to either file a complaint or to track the.
Humana Military Provider Enrollment Form Enrollment Form
Claimxten and correct coding codes with. To request reconsideration, providers have 180 days from the date a claim denied in whole, partially or recoupment date of a claim or the. Reconsideration requests are an option for providers on claimxten/correct coding rejects. Enter your member information to either file a complaint or to track the status. Use our online form to.
Humana Login How to Sign in to Humana Provider Account (2023) YouTube
To request reconsideration, providers have 180 days from the date a claim denied in whole, partially or recoupment date of a claim or the. Claimxten and correct coding codes with. Either you or your treating provider can file an appeal on your behalf. Use our online form to file a complaint, it's fast, easy, and secure. Reconsideration requests are an.
At The End Of This Packet Is A Form That You May Use For F Iling Your Appeal.
Appeals and disputes for finalized humana medicare, medicaid or commercial claims can be submitted through availity’s secure provider. Use our online form to file a complaint, it's fast, easy, and secure. If you are a participating provider and disagree with our determination after we respond to your initial online, mail or phone submission, you can. Claimxten and correct coding codes with.
Appeals And Disputes For Finalized.
Reconsideration requests are an option for providers on claimxten/correct coding rejects. Either you or your treating provider can file an appeal on your behalf. To request reconsideration, providers have 180 days from the date a claim denied in whole, partially or recoupment date of a claim or the. Enter your member information to either file a complaint or to track the status.