Caresource Prior Authorization Form - Prior authorization is how we decide if the health services will be covered by the caresource plan. If you are unsure whether or not a prior authorization is required, please refer to health partner policies or the prior authorization page on the caresource website. Please submit a separate claim recovery refund. *in order to process this request, please complete all boxes completely. The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. This facsimile and any attached document are confidential and are intended for the use of individual or entity to. Caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits.
Caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Please submit a separate claim recovery refund. This facsimile and any attached document are confidential and are intended for the use of individual or entity to. *in order to process this request, please complete all boxes completely. The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. Prior authorization is how we decide if the health services will be covered by the caresource plan. If you are unsure whether or not a prior authorization is required, please refer to health partner policies or the prior authorization page on the caresource website.
If you are unsure whether or not a prior authorization is required, please refer to health partner policies or the prior authorization page on the caresource website. Caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Prior authorization is how we decide if the health services will be covered by the caresource plan. Please submit a separate claim recovery refund. *in order to process this request, please complete all boxes completely. The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. This facsimile and any attached document are confidential and are intended for the use of individual or entity to.
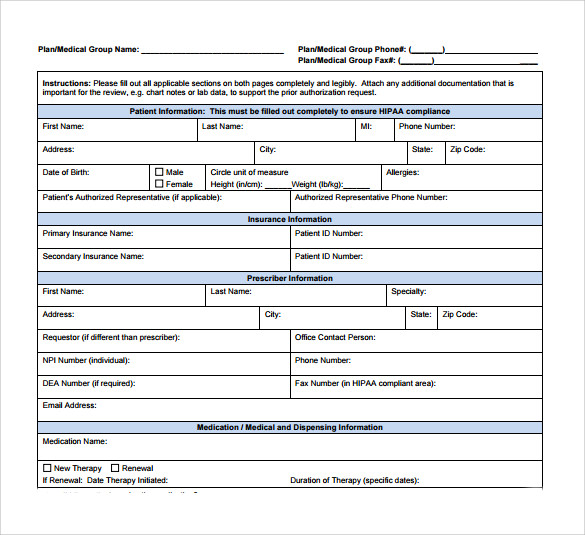
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. This facsimile and any attached document are confidential and are intended for the use of individual or entity to. *in order to process this request, please complete all boxes completely. Please submit a separate claim recovery refund. Prior authorization is.
Caresource Marketplace Prior Authorization Form
Prior authorization is how we decide if the health services will be covered by the caresource plan. The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. Caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. *in order to process this request, please complete all.
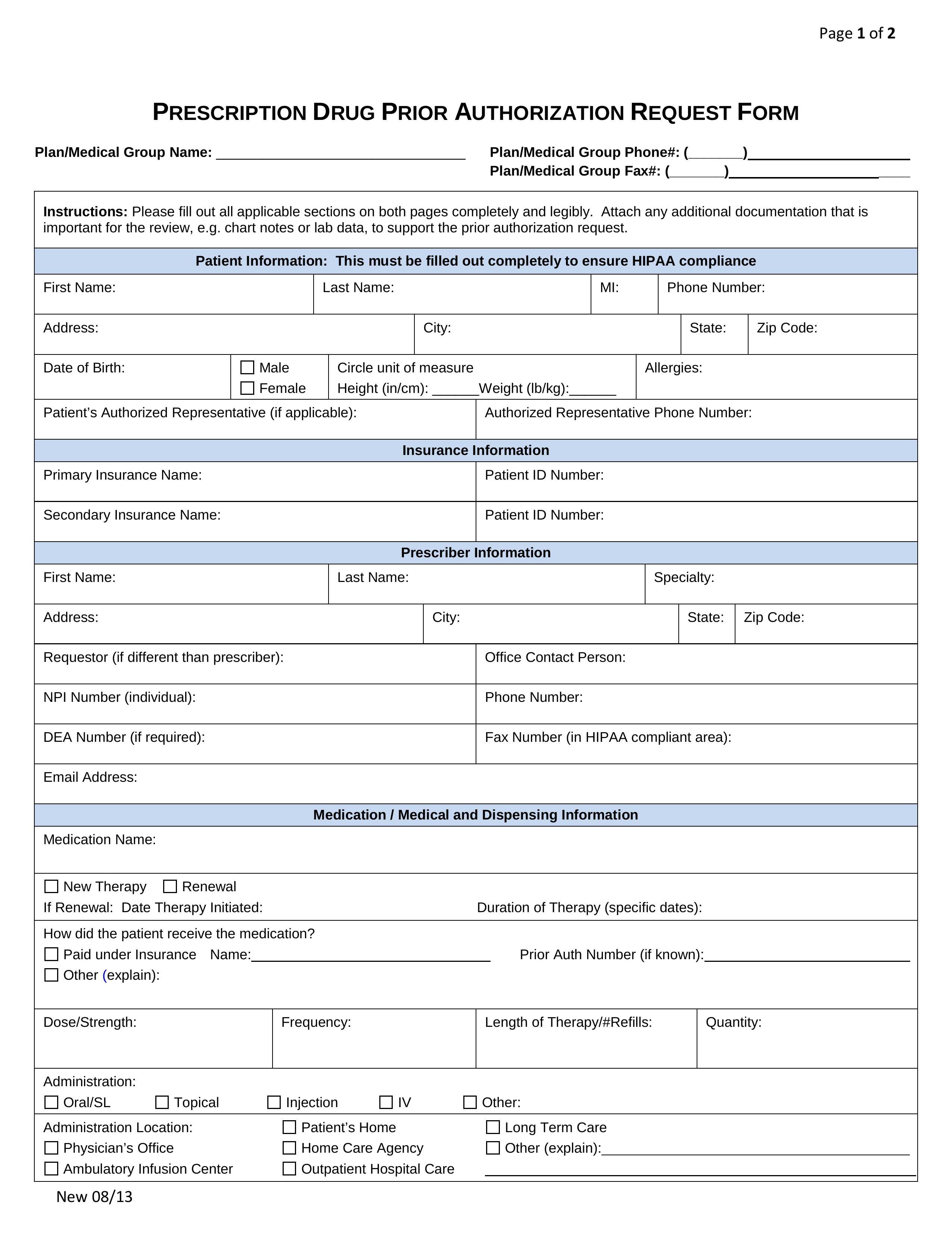
20212024 OH CareSource Medicaid Provider Prior Authorization Request
If you are unsure whether or not a prior authorization is required, please refer to health partner policies or the prior authorization page on the caresource website. This facsimile and any attached document are confidential and are intended for the use of individual or entity to. Please submit a separate claim recovery refund. The claim recovery request form has been.
Fillable Online ABA Prior Authorization Request Form CareSource Fax
This facsimile and any attached document are confidential and are intended for the use of individual or entity to. *in order to process this request, please complete all boxes completely. The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. Please submit a separate claim recovery refund. Caresource® evaluates prior.
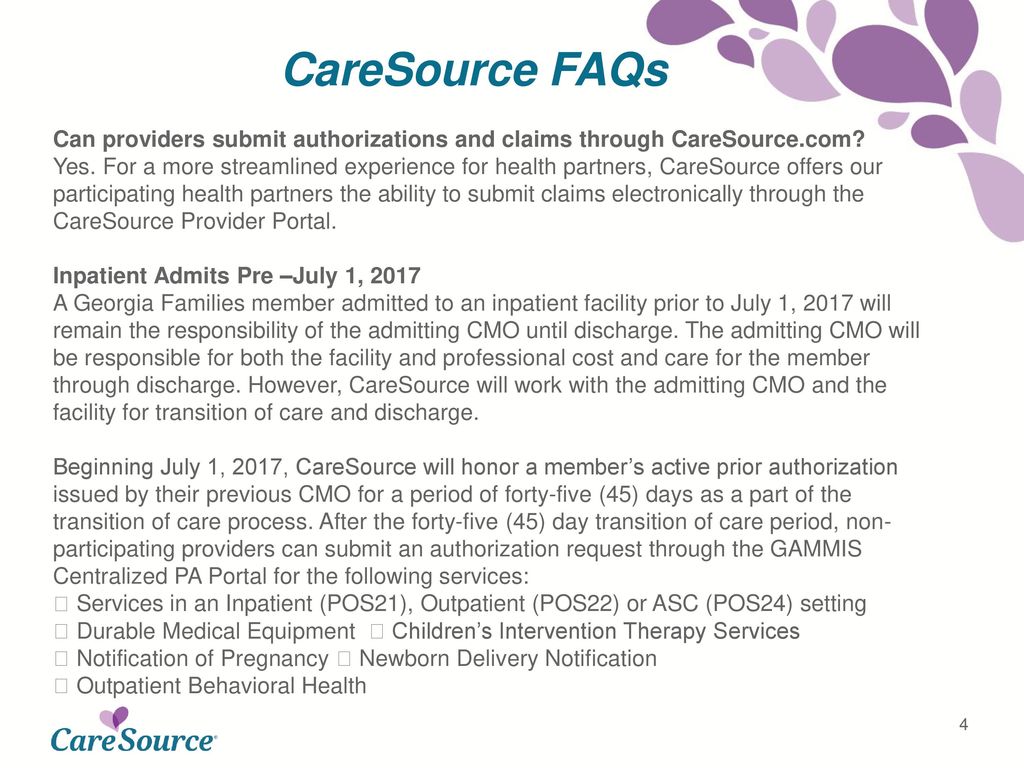
HomeTown Health Roderick M. Alexander ppt download
This facsimile and any attached document are confidential and are intended for the use of individual or entity to. *in order to process this request, please complete all boxes completely. The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. If you are unsure whether or not a prior authorization.
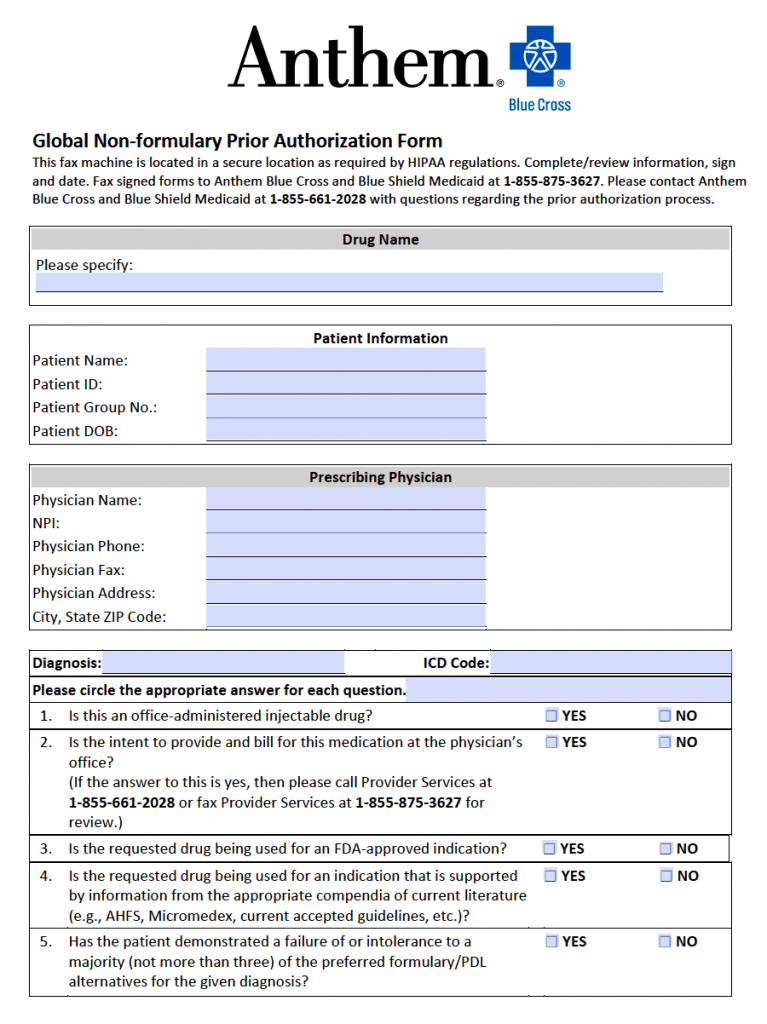
Bcbs Federal Predetermination Form at viirafaelblog Blog
If you are unsure whether or not a prior authorization is required, please refer to health partner policies or the prior authorization page on the caresource website. Caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. *in order to process this request, please complete all boxes completely. This facsimile and any attached document are confidential.
Superior Health Plan Therapy Authorization Form
The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. If you are unsure whether or not a prior authorization is required, please refer to health partner policies or the prior authorization page on the caresource website. Prior authorization is how we decide if the health services will be covered.
Fillable Online Caresource Rx Innovations Prior Authorization Form Fax
This facsimile and any attached document are confidential and are intended for the use of individual or entity to. The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. *in order to process this request, please complete all boxes completely. If you are unsure whether or not a prior authorization.
Free Prior (Rx) Authorization Forms PDF eForms
*in order to process this request, please complete all boxes completely. Please submit a separate claim recovery refund. This facsimile and any attached document are confidential and are intended for the use of individual or entity to. The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. Caresource® evaluates prior.
CareSource Medicaid Prior Authorization What Providers Need to Know
The claim recovery request form has been created to help ensure timely and accurate processing, and is available to download. If you are unsure whether or not a prior authorization is required, please refer to health partner policies or the prior authorization page on the caresource website. Prior authorization is how we decide if the health services will be covered.
The Claim Recovery Request Form Has Been Created To Help Ensure Timely And Accurate Processing, And Is Available To Download.
*in order to process this request, please complete all boxes completely. This facsimile and any attached document are confidential and are intended for the use of individual or entity to. Please submit a separate claim recovery refund. Caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits.
Prior Authorization Is How We Decide If The Health Services Will Be Covered By The Caresource Plan.
If you are unsure whether or not a prior authorization is required, please refer to health partner policies or the prior authorization page on the caresource website.